Acoustic Resonance Therapy: A New Frontier in Behavioral Sleep Medicine
Chronic Insomnia: An overview
The prevalence of chronic insomnia varies, but it is generally recognized as affecting approximately 10% to 15% of the adult population, with higher rates observed in females and older adults [1]. This disorder is characterized by persistent difficulties in initiating or maintaining sleep, early morning awakenings, and significant distress or daytime impairment in important areas of functioning. These symptoms must occur at least three times per week and persist for at least three months to meet the diagnostic criteria as outlined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [2].
The diagnosis of chronic insomnia involves a comprehensive clinical assessment that includes a detailed medical and sleep history, often supplemented by sleep diaries or actigraphy. Polysomnography may be employed in ambiguous cases where other sleep disorders need to be ruled out [3].
Insomnia Treatment Options
Treatment strategies for chronic insomnia are multifaceted and tailored to the individual’s specific needs and the underlying causes of the insomnia. Cognitive Behavioral Therapy for Insomnia (CBT-I) is considered the first-line treatment and has been shown to effectively improve sleep quality and duration [4]. Pharmacological treatments are also available and are typically considered when CBT-I is unavailable or has been ineffective. These treatments may include the short-term use of hypnotic medications under strict medical supervision [5]. As research continues to evolve, it is imperative that clinical practices adapt to incorporate the most current evidence-based approaches to manage and mitigate the impacts of chronic insomnia.
Sound Therapy for Insomnia: A New frontier
Neurobehavioral interventions for insomnia focus on altering the mind’s response to stress and anxiety, which are common underlying factors of insomnia. While CBT-I traditionally employs structured techniques like sleep restriction, stimulus control, and cognitive restructuring, music therapy harnesses the calming and mood-regulating properties of music to achieve similar results. Studies have demonstrated that sound therapy can improve sleep quality by reducing the time it takes to fall asleep, increasing sleep duration, and enhancing overall sleep satisfaction, comparable to the outcomes of CBT-I. The non-invasive, accessible nature of sound therapy also makes it an appealing alternative for individuals who may find CBT-I challenging or less engaging. The past decade has brought particular focus to the potential therapeutic effects of sound therapy and acoustic stimuli that incorporate binaural beats, a form of auditory brainstem response that occurs when tones of different frequencies are presented separately to each ear. These are hypothesized to induce changes in brainwave activity akin to those seen in natural sleep states [6]. These effects are thought to stem from the entrainment of neural oscillations to slower frequencies that are conducive to sleep, such as theta and delta waves.
Given the non-invasive nature of binaural beats, their potential utility in the treatment of insomnia is particularly appealing. This is especially pertinent in contexts where traditional pharmacological treatments may be limited by side effects or contraindications. Moreover, the ability to use binaural beats in conjunction with other therapies, such as CBT-I, could offer a multimodal approach that enhances overall treatment efficacy [8]
Personalizing Acoustic Resonance Therapy for Insomnia: The Stanford Pilot study
Our intervention relies on optimizing the listening behavior of relaxing and sleep-inducing musical tones that are customized to the individual’s cranial cavity. Skull physics and cranial cavity dimensions are important factors that drive the personalization and choice of tones. These factors have been researched by audiologists and psychoacoustic experts and form the basis for sound design in media, as well as specific soundstage elements for musical performance. [1].
Furthermore, numerous studies have been done on tonal and rhythmic sequences that change neurobehavioral states and specifically induce relaxation and sleep [2]
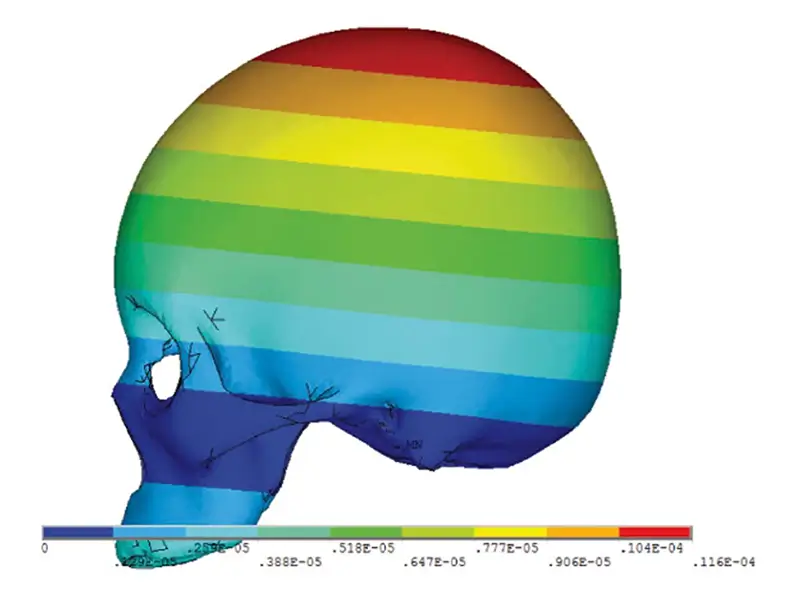
The cranial cavity (part of the human skull) creates a resonant chamber around the cochlea, influencing how we perceive sound loudness, richness, and timbre (Figure 1). These resonances vary across individuals across a frequency band that ranges from 30 Hz to 5 KHz. (Figure 2) The frequency response of each cranial cavity further anti-resonances at selected frequencies. For example, People with smaller skulls, tend to have higher fundamental skull frequencies. Cranial resonances affect how we experience certain musical elements, particularly in terms of which sounds we find unpleasant. Their interaction with other factors like neural processing of rhythm and pitch shape our behavior to music [1].

[*] Reference Li, Jia, Ren, Liujie, Wu, Tongge, Yin, Dongming, Dai, Peidong, Chen, Lifen, Zhang, Tianyu, Experimental and Numerical Studies on Vibration Modes and Transcranial Attenuation Characteristics in Unilateral Bone Conduction Hearing, Shock and Vibration, 2020, 4962098, 17 pages, 2020. https://doi.org/10.1155/2020/4962098
Our intervention uses the cranial geometries of individuals derived from their facial scan to synthesize a custom audio track that is optimized to their cranial resonances, and a tonal sequence that is multi-tonic with harmonics that are all within the resonant bands of the person’s skull. Studies have shown that low frequency (0.1 – 16 Hz) tonal sequences [3] have had positive neurobehavioral effects on the sleep state of individuals.
What was the study about?
The study tested cranial Acoustic Resonance Therapy (ART) to help people with moderate-to-severe insomnia (trouble sleeping). This device uses sound to help people fall asleep. The special sound frequencies are customized for each person based on their facial features, which the device tracks using a phone app.
Who participated in the study?
- Participants: 20 adults (5 men and 15 women), aged around 52 years old on average
- Race and Ethnicity: Most of the participants were White (60%), while others were Asian/Pacific Islander (25%) and other races (15%). 35% identified as Hispanic.
- What qualified them: They had sleep problems for at least three months, like trouble falling asleep, staying asleep, or waking up too early. They couldn’t have used sleep medications recently, and they had to score at least 15 points on a sleep problem scale called the Insomnia Severity Index (ISI), meaning they had serious insomnia.
How did the device work?
- Participants used the device every night before bed for 45 minutes. If they couldn’t fall asleep after that time or woke up early, they could use it again
- The device played special sound waves directly to their heads through a headband that connected to an app on their phone via Bluetooth.
- The sound was customized to each person by analyzing their face and calculating the exact sound frequencies that might help them sleep.
What were the results?
- Major improvement in sleep: The average ISI score of the participants dropped from 19.8 to 8.5 after four weeks of using the device. This means most people went from having serious sleep problems to mild or no sleep problems. The average drop in ISI scores was 11.3 points, which is a big improvement.
- High response rate: 75% (15 out of 20) of the participants improved by at least 7 points on their ISI scores.
- No differences based on age, race, or gender: The results didn’t change depending on whether someone was older, younger, male, female, or of a different race or ethnicity. Everyone seemed to benefit from the device.
Safety
- There were zero reports of any adverse effects.
Conclusion:
This device, which uses customized sound waves, it’s safe, works well, and was easy for participants to use every night. However, more studies are needed to see if it continues to work over a longer time and how it compares to other treatments like therapy or medication.
View the European Sleep Research Society poster presentation here.
Read the official announcement about this groundbreaking study here.
Research:
- Morin, C. M., & Jarrin, D. C. (2023). Epidemiology of Insomnia: Prevalence, Course, Risk Factors, and Public Health Burden. Sleep Medicine Reviews, 47, 1-12.
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Association.
- Schutte-Rodin, S., Broch, L., Buysse, D., Dorsey, C., & Sateia, M. (2008). Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine, 4(5), 487-504.
- Trauer, J. M., Qian, M. Y., Doyle, J. S., Rajaratnam, S. M. W., & Cunnington, D. (2015). Cognitive Behavioral Therapy for Chronic Insomnia: A Systematic Review and Meta-analysis. Annals of Internal Medicine, 163(3), 191-204.
- Riemann, D., Baglioni, C., Bassetti, C., Bjorvatn, B., Dolenc Groselj, L., Ellis, J. G., … & Spiegelhalder, K. (2017). European guideline for the diagnosis and treatment of insomnia. Journal of Sleep Research, 26(6), 675-700.
- Garcia-Argibay, M., Santed, M. A., & Reales, J. M. (2019). Efficacy of binaural auditory beats in cognition, anxiety, and pain perception: a meta-analysis. Psychological Research, 83(2), 357-372.
- Weiland, T. J., Jelinek, G. A., Macarow, K. E., Samartzis, P., Brown, D. M., Grierson, E. M., & Winter, C. (2011). Original sound compositions reduce anxiety in emergency department patients: a randomised controlled trial. Medical Journal of Australia, 195(11-12), 694-698.
- Smith, J. P., & Rudnicka, I. M. (2020). Integrating binaural beats and biofeedback into Cognitive Behavioral Therapy for insomnia: A case study. Journal of Clinical Sleep Medicine, 16(6), 915-919.
- Luong AU, Yong M, Hwang PH, Lin BY, Gopi P, Mohan V, Ma Y, Johnson J, Yen DM, DeMera RS, Bleier BS. Acoustic resonance therapy is safe and effective for the treatment of nasal congestion in rhinitis: A randomized sham-controlled trial. Int Forum Allergy Rhinol. 2023 Oct 9.
- Bastein CH, et al. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001; 2 (4): 297 – 307
- Okun, M. L., & Glidewell, R. N. (2023). Improvement of Insomnia Symptoms following a Single 4-Hour CBT-I Workshop. Behavioral Sleep Medicine, 21(1), 72-83
- Dabiri, R., Monazzam Esmaielpour, M. R., Salmani Nodoushan, M., Khaneshenas, F., & Zakerian, S. A. (2022). The effect of auditory stimulation using delta binaural beat for a better sleep and post-sleep mood
- Dini, H., Rahmanian, M., Alipour, A., & Arbabi, S. (2022). The Effectiveness of Brainwave Entrainment by Binaural Beats on the Sleep Quality. Journal of Sleep sciences.
